Introduction of the HPV Vaccine in Nepal - 2008
HPV Vaccination – Gardasil
(Gardasil is quadrivalent vaccine that protects against four strains of HPV HPV 16 &18 – causing approx 75% of cervical cancer cases HPV 6 & 11 – causing approx 90% of genital warts Gardasil can also protect against vaginal and vulvar cancer. Gardasil does not protect against cervical cancer and diseases caused by other HPV strains. Therefore, even with the use of the vaccine, routine screening is essential )
Gardasil information
(The Gardasil vaccine is most effective when administered between ages 9 to 26 years. Vaccine administered intramuscularly into upper arm. Three doses are required for vaccine to be effective. 1st dose, 2nd dose given 2 months after 1st dose, 3rd dose given 4 months after the 2nd Side effects are uncommon but include pain, swelling, itching, bruising and redness at the injection site. Headache, fever, nausea, dizziness, vomiting and fainting have also been observed)
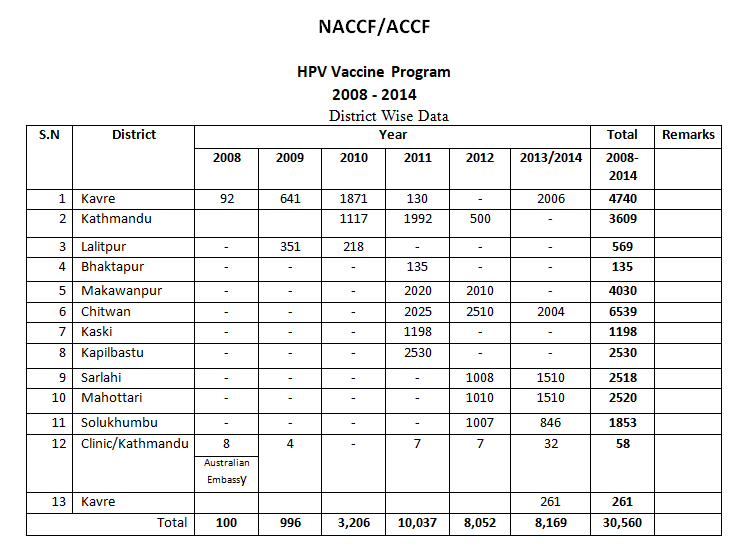
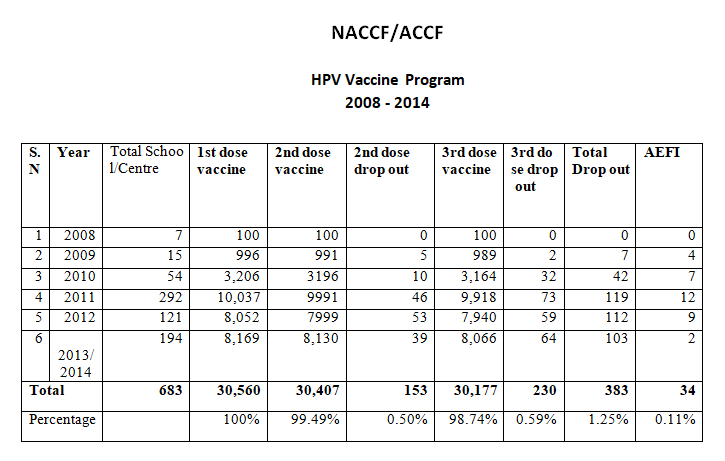
HPV Vaccine school-based program 2008-2014
The Gardasil HPV vaccine was introduced in Nepal in 2008 and implemented by the Nepal Australian Cervical Cancer Foundation (NACCF) and supported by the AXIOS Gardasil Access Program (GAP) USA, Australian Cervical Cancer Foundation (ACCF), Australian Himalayan Foundation (AHF)

Program Design
- Family Health Division (FHD) communicates official program information to the district level government agencies to encourage support
- Contact made with the public, community, private schools and their associations to reach girls, parents/guardians
- Community meetings set up as an interactive environment for school administrators to provide information and teach girls and their parents about the vaccine
- Girls asked to bring back signed consent forms to school prior to the day of first vaccination.
Administration Sites
Schools were selected as the key administration site for several reasons:
1. Maximum numbers of girls are accessible through schools
2. Schools provide a convenient way to run vaccine awareness programs for students, teachers and parents with easy follow-up
3. Schools provide better chance for higher compliance
4. A coordinator for the vaccine project was nominated by the school administration in each school
Acknowledgments
Partners
- Government Involvement
- Vaccine program approval was granted by the Ministry of Health and Population (MoHP)
- Monitoring of district level program implementation was done by Family Health Division (FHD)
Local Partners
- Government District Health Offices (DHO):
- DHO Makwanpur district
- DHO Kapilbastu District
- BPKM Cancer Hospital (Government Cancer Hospital) Chitwan
- Private Pharmaceuticle Co. (Yetichem) at Kathmandu to provide main cold chain management needs at no cost
- Other district level Government agencies and
- NGOs at Kaski, Kathmandu, Bhaktapur , Lalitpur , Kavre , RRPC Sarlashi, RYC , Mohottari, REED Nepal ,Solukhumbu
International Partners
- Australian Cervical Cancer Foundation (ACCF) Brisbane provided financial and institutional support for local management
Axios-managed Gardasil Access Program provided Gardasil through a pledge from Merck and Co.
HPV Vaccine program implementation
Total Vaccinated girls : 30,560
Target group : 11 to 13 age group
Vaccinated District : Kavre, Kathmandu, Lalitpur, Bhaktapur, Makawanpur, Chitawan, Kaski, Kapilbastu, Sarlahi, Mahottari, Solukhumbu
Program Successes
Prior to the introduction of HPV Vaccine in Nepal in 2008, knowledge of vaccine was extremely limited. Now, awareness has risen dramatically across Nepal. Safely delivered vaccination to 30,560 girls in the target group of 11-13 years of age. No record of life threatening AEFI for recipients. Gardasil vaccine now available on the Nepali drug-store market. Information material has been developed in Nepali. Had success (although still a challenge) in overcoming bureaucratic, social and cultural barriers.
Overcoming Challenges – what is needed…
- Active cooperation from school administrations, to encourage compliance as well as increased awareness and education through local and national media in the hope of minimizing skepticism amongst the community, school girls and their parents.
- The World Health Organization to more actively provide publicity to clear misinformation on vaccine projects as ‘new’ or ‘experimental’.
Lessons Learned & Challenges
The awareness of HPV and/or cervical cancer morbidity and mortality is still very low in urban areas and almost zero in rural areas. Very little knowledge of HPV vaccine or other vaccines. Focus amongst Nepalese people still on treatment of immediate health problems rather than prevention. Benefit is not seen until years after immunization
Concern on HPV vaccination as a ‘new’ or ‘experimental’ program.
School administrations are often hesitant to run vaccine program due to:
- Concerns about any adverse reactions that may arise and who will be responsible
- Limited knowledge of the HPV vaccine, including benefits and safety profile
- Concerns over not having enough time to conduct the program
Follow-up for 2nd and 3rd doses became challenging without active cooperation of the school administration
For that reason, schools were encouraged to keep detailed follow-up information in a computerized database at NNCTR in Banepa following each vaccination round
– The cost of the vaccine is sometimes a barrier
– The Government’s position regarding the vaccine is not clear
– There are inadequate resources
– Ensuring the maintenance of vaccine quality under cold chain methods
– There are challenges associated with full compliance and timing
– The percentage of drop outs in the 2nd and 3rd doses can be high for many reasons such as absentees, illness and others.
Conclusion
- 30,560school girls of 11 to 13 age group have vaccinated through the NACCF vaccination program.
- A comprehensive Cervical Cancer Prevention Program inclusive of Cervical cancer education, Cervical Cancer Screening and HPV Vaccination is the need of the day in women health services of the country.
The HPV vaccination and screening programs run by the NACCF/NNCTR only touch the tip of the iceberg. There are many, many girls who have yet to be vaccinated.